Type 2 Diabetes Mellitus
Diabetes is the most common chronic metabolic disease and a major source of morbidity and mortality. Type 2 diabetes mellitus (T2DM) is the most prevalent form, accounting for around 90 per cent of cases worldwide. Figures released by the International Diabetes Federation (IDF) in December 2021 show that more than half a billion adults globally are living with diabetes. This is a rise of 16 per cent (74 million) since the previous IDF estimates in 2019. Worldwide, 537 million adults aged 20-79 years are living with diabetes, and 541 million adults have pre-diabetes, which places them at high-risk of developing T2DM. The prevalence of diabetes worldwide is growing at an alarming rate, and is predicted to rise to 643 million by 2030, and 784 million by 2045. The diabetes epidemic is unfolding because of increasing obesity rates, sedentary lifestyles and an ageing population.
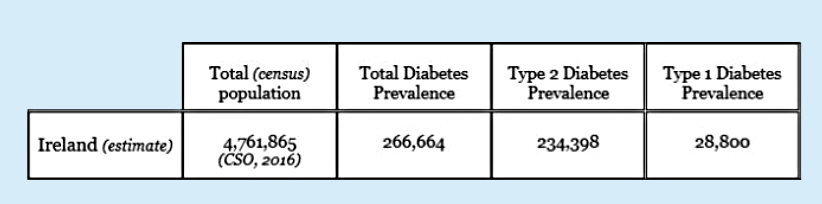
TABLE 1: Diabetes prevalence in Ireland. Source: Diabetes Ireland. Available at: www.diabetes.ie/about-us/diabetes-in-ireland/
There is still no National Diabetes Registry in Ireland, therefore national estimates are not fully accurate. The figures provided by Diabetes Ireland (Table 1, January 2022) use data modelled from the Scottish Diabetes Register. In Scotland, the prevalence of diabetes was 5.6 per cent of the total census population in 2020. Table 1 estimates the total diabetes prevalence in Ireland at approximately 266,664 people. The prevalence of T2DM is estimated at 234,398 people (87.9 per cent of the total diabetes population) and type 1 diabetes at 28,800 (10.8 per cent of the total diabetes population), based on the Scottish prevalence. The true prevalence of T2DM in Ireland, however, is likely to be higher, as hyperglycaemia develops gradually, and at the early stage many cases go undiagnosed.
According to the 2015 Irish Longitudinal Study on Ageing (TILDA), 10 per cent of adults aged 50 and over in Ireland have T2DM, rising to 16 per cent in those aged 80 and over. The TILDA study revealed that 1:10 people with diabetes in this population are undiagnosed, and that a further 5.5 per cent of the older population have pre-diabetes, which puts them at an increased risk of developing T2DM in the future. The study also found that T2DM is more common in men (12 per cent) than women (7 per cent), and those with a self-reported history of hypertension, high cholesterol, and being centrally obese, while having low levels of physical activity also has a strong correlation with both diabetes and pre-diabetes.
The IDF Atlas 2021 ranked Ireland seventh in the world for diabetes-related health expenditure per person. The economic burden of diabetes on the Irish healthcare system is a major challenge for Government and the HSE. National estimates comparing health-service use between people over 50 years of age with and without diabetes (2009-2011) show that diabetes was associated with an 87 per cent increase in outpatient visits, a 52 per cent increase in hospital admissions, and a 33 per cent increase in emergency department attendances.
TABLE 2: Criteria for testing for diabetes in asymptomatic adults. Source: ICGP (2016)
The CODEIRE study (2006) stated that costs associated with diabetes in Ireland consume between 4-to-6 per cent of annual healthcare expenditure. If the same percentage (4-to-6 per cent) was to be applied to the Irish healthcare expenses in 2019, the costs associated with diabetes would have been as high as €1.2 billion to €1.4 billion, with approximately 50 per cent of the costs associated with hospitalisations and treatment of complications. With the growing prevalence of diabetes in Ireland, comprehensive economic data is required to ensure that appropriate resources are allocated to the management of the disease.
Pathophysiology
T2DM is an insulin-resistance condition with associated beta-cell dysfunction. It occurs when blood glucose levels are too high (hyperglycaemia) due to insufficient insulin production, or when the insulin that is produced by the pancreas is not working effectively. T2DM results from an interaction between genetic and environmental factors, and ranks high on the international health agenda as a global pandemic, and as a threat to human health and global economies.
In T2DM, the response to insulin is diminished, and this is defined as insulin resistance. During this state, insulin is ineffective and is initially countered by an increase in insulin production to maintain glucose homeostasis. However, as the disease progresses, beta cells change and insulin secretion is unable to maintain glucose homeostasis, producing hyperglycaemia, resulting in T2DM.
T2DM is most commonly seen in people over the age of 40. However, it is also now increasingly seen in children, adolescents, and younger adults due to rising levels of obesity, physical inactivity, and energy-dense diets. Most patients with T2DM are obese or have a higher body fat percentage, distributed predominantly in the abdominal region. This adipose tissue promotes insulin resistance through various inflammatory mechanisms, including increased FFA release and adipokine dysregulation. Lack of physical activity in people with hypertension or dyslipidaemia also increases the risk of developing T2DM.
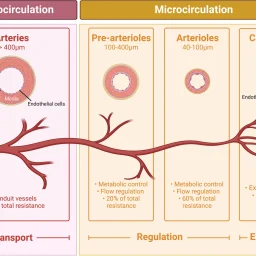
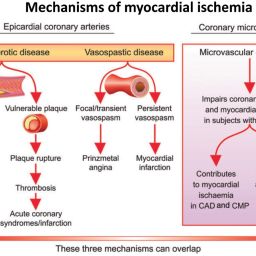
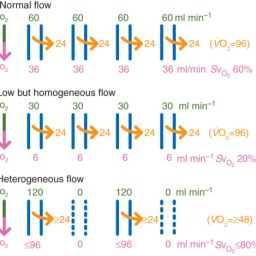
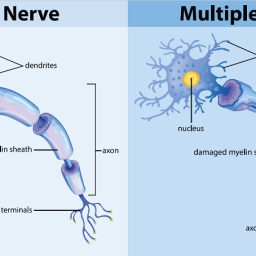
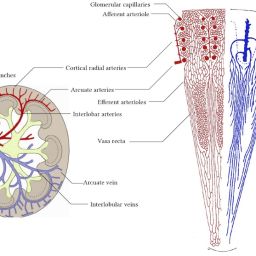
Chronic hyperglycaemia can cause damage to various organ systems, leading to the development of disabling and life-threatening health complications, most prominent of which are microvascular (retinopathy, nephropathy, and neuropathy) and macrovascular complications, leading to a two-to-four-fold increased risk of cardiovascular disease.
Important Takeaway:
Damage to the mitochondria, the structures that generate energy within cells, plays a key role in the progression of metabolic diseases, and Imeglimin protects mitochondria from damage.
For the full article, please visit the following link: https://www.medicalindependent.ie/clinical-news/endocrinology/type-2-diabetes-mellitus/
By Priscilla Lynch – 26th Apr 2022
Frequently Asked Questions
What is Type 2 Diabetes Mellitus?
Type 2 Diabetes Mellitus is a chronic condition that affects the way the body processes blood sugar (glucose). It occurs when the body becomes resistant to insulin or when the pancreas fails to produce sufficient insulin.
What are the risk factors for Type 2 Diabetes?
Risk factors include obesity, physical inactivity, poor diet, family history, and age. Additionally, conditions such as high blood pressure and high cholesterol can increase the risk.
How is Type 2 Diabetes managed?
Management includes lifestyle changes such as a healthy diet and regular physical activity, monitoring blood sugar levels, and medications as prescribed by a healthcare provider.
Physical Vascular Therapy in Practice – Scientific Evidence and Therapeutic Applications
Learn more about the scientific evidence and therapeutic applications of physical vascular therapy: