Comprehensive list of illnesses related to microcirculation
Our exploration of how microcirculation affects health aims to broaden understanding of this crucial, yet often overlooked, area. Join us as we uncover the significant role of these tiny blood vessels on well-being.
This is a comprehensive list of illnesses or conditions related to microcirculation.
- Sepsis
- Septic shock
- Cardiogenic shock
- Hypovolemic shock
- Hemorrhagic shock
- Ischemic heart disease
- Myocardial infarction
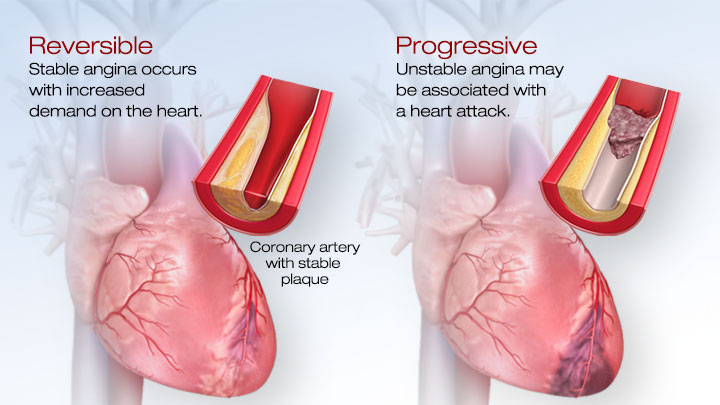
- Angina pectoris
- Coronary artery disease
- Peripheral artery disease
- Arteriosclerosis
- Atherosclerosis
- Diabetes mellitus (especially diabetic microvascular complications)
- Hypertension
- Hypotension
- Chronic kidney disease
- Renal artery stenosis
- Renal microvascular disease
- Renal failure
- Renovascular hypertension
- Raynaud’s disease
- Raynaud’s phenomenon
- Thromboangiitis obliterans (Buerger’s disease)
- Ischemic stroke
- Hemorrhagic stroke
- Transient ischemic attack (TIA)
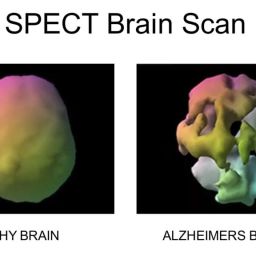
- Cerebral microangiopathy
- Acute respiratory distress syndrome (ARDS)
- Pulmonary embolism
- Pulmonary hypertension
- Chronic obstructive pulmonary disease (COPD)
- Asthma
- Chronic bronchitis
- Emphysema
- Sickle cell disease
- Thrombotic microangiopathies (e.g., thrombotic thrombocytopenic purpura, hemolytic uremic syndrome)
- Vasculitis (e.g., giant cell arteritis, Takayasu’s arteritis)
- Kawasaki disease
- Microvascular angina
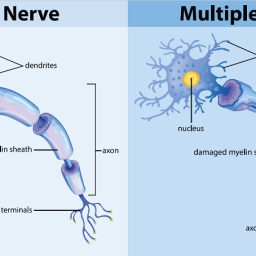
- Peripheral neuropathy
- Diabetic neuropathy
- Diabetic retinopathy
- Macular degeneration
- Chronic venous insufficiency
- Deep vein thrombosis (DVT)
- Varicose veins
- Lymphedema
- Erythromelalgia
- Frostbite
- Gangrene
This list covers a wide range of illnesses and conditions where microcirculation plays a significant role in their pathophysiology.
The microcirculation is the motor of sepsis.
By Can Ince. Article number: S13 (2005) Re-establishing organ function in severe sepsis: targeting the microcirculation.
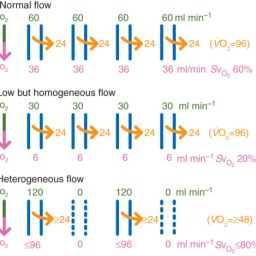
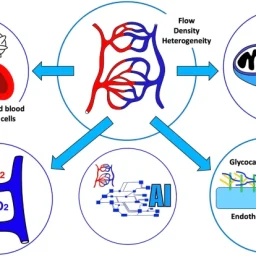
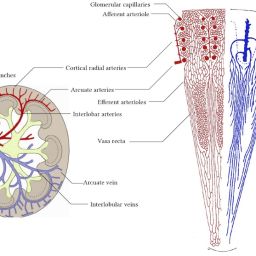
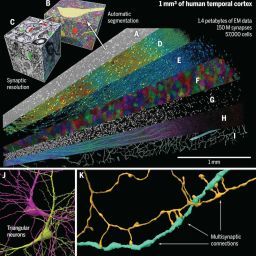
The microcirculation is vital for delivering oxygen and nutrients to tissues, supporting immune function, and transporting drugs in diseases. It consists of tiny blood vessels like arterioles, capillaries, and venules, where oxygen is released to tissues. The main components are endothelial cells, smooth muscle cells (mostly in arterioles), red blood cells, white blood cells, and plasma. The microcirculation varies in structure and function across organs. Factors like pressure, muscle tone in arterioles, blood viscosity, and capillary openness mainly determine blood flow in these vessels.
Read the full study: Link: https://ccforum.biomedcentral.com/articles/10.1186/cc3753
What is Cardiogenic shock?
Cardiogenic shock is a life-threatening condition that occurs when the heart suddenly cannot pump enough blood to meet the body’s needs. It is often caused by a heart attack or heart failure, leading to inadequate blood flow to the body’s organs, which can result in organ failure and even be fatal. Symptoms of cardiogenic shock include fatigue, rapid heartbeat, shortness of breath, hypotension, sweating, chest pain, dizziness, nausea, and decreased level of consciousness.
Prompt treatment is crucial in cardiogenic shock, with interventions aimed at improving blood flow to the body, such as opening blocked heart arteries or using medications to enhance the heart’s pumping ability. In severe cases, advanced options like mechanical support devices or heart transplantation may be necessary.
Despite advances in treatment, cardiogenic shock remains a serious condition with high mortality rates, emphasizing the importance of early diagnosis and intervention to improve outcomes.

Symptoms Causes: Link: https://www.mayoclinic.org/diseases-conditions/cardiogenic-shock/symptoms-causes/syc-20366739
What are the stages of cardiogenic shock? – Link: https://my.clevelandclinic.org/health/diseases/17837-cardiogenic-shock
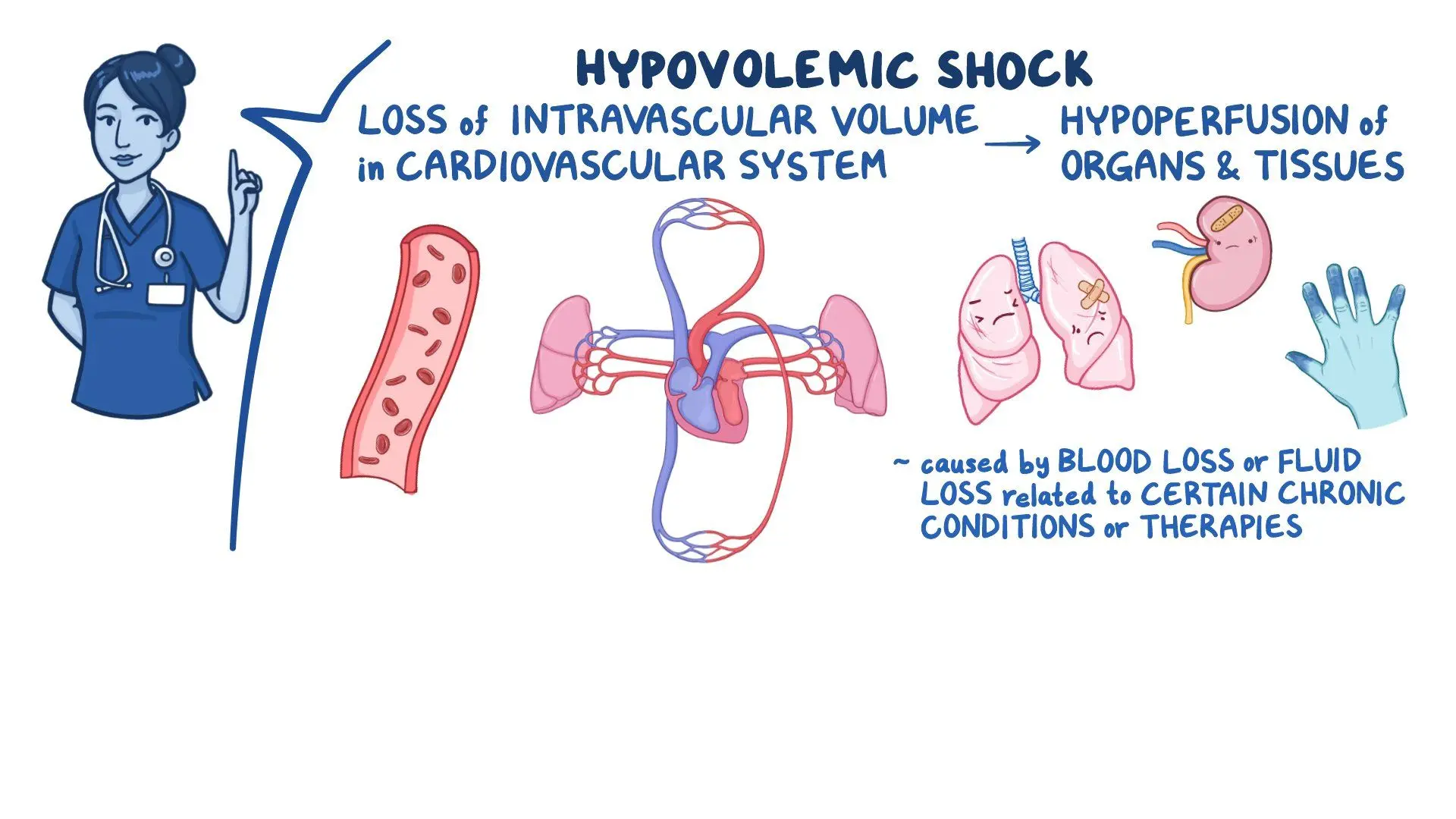
What is Hypovolemic shock?
Hypovolemic shock is a critical medical emergency that occurs when the body loses a significant amount of blood or fluids, leading to the heart’s inability to pump enough blood to meet the body’s needs. This condition can result from various causes such as severe bleeding from injuries, internal bleeding, burns, excessive sweating, diarrhea, or vomiting.
The symptoms of hypovolemic shock can include anxiety, cool and clammy skin, confusion, rapid breathing, pale skin color, rapid heart rate, sweating, and unconsciousness. The severity of symptoms correlates with the extent and speed of blood or fluid loss. Hypovolemic shock progresses through stages based on the percentage of blood volume lost, ranging from mild to severe, with each stage exhibiting distinct symptoms and vital signs changes.
Prompt medical attention is crucial in treating hypovolemic shock, focusing on stabilizing blood volume levels, stopping fluid loss, and addressing the underlying cause. Treatment may involve intravenous fluids, blood transfusions, and managing complications like organ failure.
Older adults are particularly vulnerable to hypovolemic shock, emphasizing the importance of early recognition and intervention to improve outcomes and prevent complications.
Link to article: Link: https://emedicine.medscape.com/article/760145-overview?form=fpf
Link to article: Link: https://medlineplus.gov/ency/article/000167.htm
What is Hemorrhagic shock?
Hemorrhagic shock is a severe and life-threatening medical emergency that occurs due to heavy blood loss, either internally or externally. This type of shock is a subset of hypovolemic shock, where the body’s blood volume decreases significantly, leading to inadequate oxygen delivery to tissues and organs. Hemorrhagic shock can result from various causes such as severe trauma, deep cuts, gunshot wounds, amputations, or severe burns. When heavy bleeding occurs, essential substances like oxygen are lost faster than they can be replaced, causing organs to shut down.
Symptoms of hemorrhagic shock include blue lips and fingernails, low urine output, excessive sweating, shallow breathing, dizziness, confusion, chest pain, low blood pressure, rapid heart rate, weak pulse, anxiety, and a sense of impending doom. The severity of hemorrhagic shock is classified into four classes based on the percentage of blood volume lost, ranging from mild to severe.

Immediate medical attention is crucial in treating hemorrhagic shock, focusing on stopping the bleeding, restoring blood volume through IV fluids and blood transfusions, and using vasopressors to increase blood pressure. Prompt treatment is essential to prevent complications like organ damage, gangrene, and death, with the recovery outlook depending on the extent of blood loss and preexisting health conditions.
Link to article: Link: https://www.healthline.com/health/hemorrhagic-shock
Link to article: Link: https://www.ncbi.nlm.nih.gov/books/NBK470382/
What is Ischemic heart disease?
Ischemic heart disease refers to heart damage caused by poor blood flow to the heart, usually resulting from coronary artery disease. This condition occurs when the coronary arteries narrow, leading to reduced blood flow to the heart muscle. Ischemic heart disease can also be known as cardiac ischemia or ischemic cardiomyopathy.
As the heart weakens due to reduced blood flow, it may lead to complications such as blood clots, heart valve disease, heart failure, abnormal heart rhythms (arrhythmia), and other issues. Symptoms may not be present initially, and for some individuals, the first sign of ischemic heart disease could be a heart attack.
Treatment for ischemic heart disease focuses on restoring blood flow and reducing the risk of heart attacks, with options ranging from lifestyle changes and medications to minimally invasive or surgical procedures like PCI (percutaneous coronary intervention) or CABG (coronary artery bypass grafting).
Link to article: Link: https://www.advocatehealth.com/health-services/advocate-heart-institute/conditions/ischemic-heart-disease
Link to article: Link: https://www.heart.org/en/health-topics/heart-attack/about-heart-attacks/silent-ischemia-and-ischemic-heart-disease
Link to article: Link: https://www.nhs.uk/conditions/coronary-heart-disease/