Clinical Manifestations of Disordered Microcirculatory Perfusion in Severe Sepsis
By Stephen Trzeciak and Emanuel P Rivers
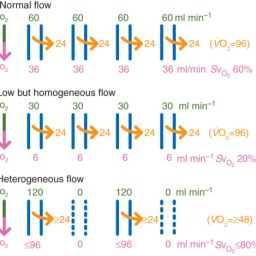
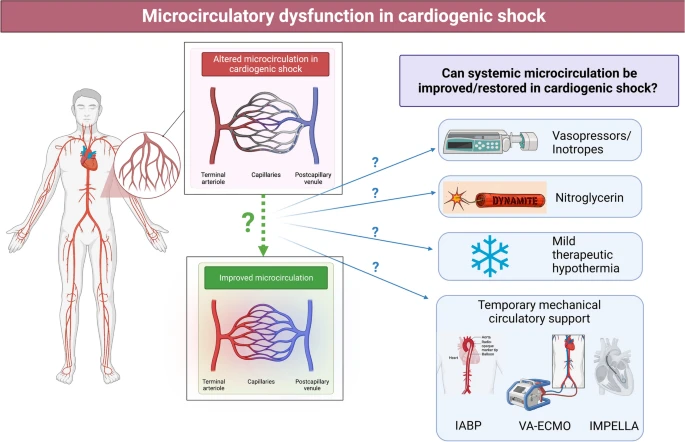
This study examines the potential impact of novel therapies on microcirculatory blood flow in sepsis, focusing on vasodilator agents. It suggests that the microcirculation could be a promising target for new treatments, especially if traditional markers of resuscitation effectiveness fail to normalize despite achieving goals for upstream endpoints.
Clinical studies have shown that vasodilators like prostacyclin, nitroglycerin, and dobutamine can improve microcirculatory blood flow in septic shock patients. However, their clinical impact remains uncertain, and their use has been limited due to side effects such as arterial hypotension.
Can vasodilators like prostacyclin, nitroglycerin, and dobutamine improve microcirculation?
Yes, vasodilators such as prostacyclin, nitroglycerin, and dobutamine have been shown in clinical studies to potentially improve microcirculatory blood flow in septic shock patients. These vasodilators work through different mechanisms to dilate blood vessels, leading to improved perfusion. However, the overall clinical impact and safety require further research.
What are the side effects of prostacyclin, nitroglycerin, and dobutamine?
Prostacyclin (PGI2)
- Can induce or worsen hypotension (low blood pressure).
- May cause flushing and headaches.
- Poor tolerance in some patients due to hypotensive effects.
Nitroglycerin
- Causes vasodilation, which may lower blood pressure.
- Side effects: headache, dizziness, flushing.
- Can trigger reflex tachycardia (increased heart rate).
Dobutamine
- Acts as an inotropic agent with vasodilatory effects.
- Side effects: tachycardia, palpitations.
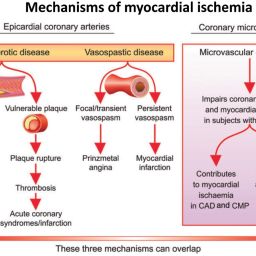
- Possible arrhythmias and myocardial ischemia in some patients.
Read the full study here:
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3226160/